Research AKI, AGMA, septic ATN, Nephrotoxins, is Covid 19 related to AKI?
1) Acute Kidney Injury
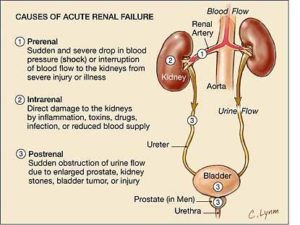
AKI is characterized by an abrupt decrease in renal function. The etiology can be classified into prerenal, intrinsic renal, and postrenal causes. Prerenal disease and acute tubular necrosis (ATN), together account for approximately 65 to 75 percent of cases of AKI.
AKI can be defined as one or more of three criteria:
1) A rise in serum creatinine of at least 0.3 mg/dL (26.5 micromol/L) over a 48-hour period and/or
2) A rise in serum creatinine ≥1.5 times the baseline value within the seven previous days
3) A urine volume ≤0.5 mL/kg per hour for six hours.
AKI can result in decreased acid excretion with retention of nitrogen waste products and increased bicarb excretion. With prolonged and/or severe ischemia, Acute tubular necrosis can occur resulting in histologic and occlusion of the tubular lumen by casts and cell debris.
Diagnosis
- Increased BUN:creatinine ratio >20:1
- Fractional excretion of sodium (FENA)<1%, urine sodium <20
- Concentrated urine: high specific gravity (>1.0202) and increased osmolarity ( >500) mOsm/kg)
Treatment: The appropriate treatment is to increase renal perfusion, as with volume repletion in patients with true volume depletion.
2)Anion Gap Metabolic Acidosis
The anion gap is used in medicine to identify the cause of metabolic acidosis and a lower than normal pH in the blood. The anion gap is calculated by subtracting the serum concentrations of chloride and bicarbonate (anions) from the concentration of sodium and potassium (cations). Because potassium concentrations are very low, it has little effect on the calculated anion gap, so it is often left out of the equation.
Anion Gap = ([Na+] − ([Cl−] + [HCO−3]). Normal serum AG = 3-10 mEq/L
Metabolic acidosis is primarily a reduction in bicarbonate (HCO3−), typically with a compensatory reduction in carbon dioxide partial pressure (Pco2). In this, the pH may be markedly low or slightly subnormal. Relating to the anion gap, Metabolic acidosis are categorized as high or normal anion gap based on the presence or absence of unmeasured anions in serum discussed earlier.
Causes of Anion Gap Metabolic acidosis
High anion gap acidosis |
Normal anion gap acidosis |
| · Ketoacidosis
· Lactic acidosis · Renal failure · Toxic ingestions |
· Gastrointestinal (GI) or renal HCO3− loss
· Impaired renal acid excretion
|
Symptoms and signs
Mild cases can be asymptomatic while more severe cases can have the following:
- nausea and vomiting
- lethargy
- hyperpnea- increased depth and rate of breathing. It may be physiologic—as when required to meet metabolic demand of body tissues
Diagnosis
- Arterial blood gas (ABG) and serum electrolyte measurement.
- Labs: Glucose, BUN (blood urea nitrogen), Creatinine, Lactate, Possible toxins
Treatment
- Treat the cause (hypovolemic shock, missed hemodialysis)
- Hemodialysis: is required for renal failure and sometimes for ethylene glycol, methanol, and salicylate poisoning.
- IV sodium bicarbonate may be indicated when pH is very low(ie, pH less than 7.1)
3)Septic Acute tubular necrosis (ATN)
Septic ATN occurs due to acute tubular cell injury, prolonged ischemia and dysfunction. This can result in histologic changes, including necrosis, occlusion of the tubular lumen by casts and cell debris. The diagnosis is suspected when azotemia (abnormal high levels of nitrogen-containing compounds: urea, creatinine, body waste compounds in the blood) develops after the following causes:
- Renal hypoperfusion, most often caused by hypotension or sepsis (ischemic ATN; most common, especially in patients in an ICU)
- Nephrotoxins- Toxic agents that inhibit, damage or destroy cells/tissues of the kidneys
- Major surgery (often due to multiple factors)- Major surgery and advanced hepatobiliary disease increase the risk of aminoglycoside toxicity. Certain drug combinations (eg, aminoglycosides with amphotericin B) may be especially nephrotoxic. NSAIDs may cause several types of intrinsic kidney disease, including ATN.
4)Common nephrotoxins include the following:
- Aminoglycosides
- Amphotericin B
- Cisplatin and other chemotherapy drugs
- Radiocontrast (particularly ionic high osmolar agents given IV in volumes > 100 mL—
- NSAIDs (especially when concurrent with poor renal perfusion or other nephrotoxic agents)
- Colistimethate
- Calcineurin inhibitors (eg, cyclosporine, tacrolimus, used systemically)
- Vancomycin (particularly with supratherapeutic dosing)
Sepsis — Endotoxemia may play an important role in AKI and this is observed as part of the multiple organ dysfunction syndrome. Among the critically ill, sepsis is the most common cause of AKI. The mechanism by which endotoxemia leads to AKI is incompletely understood.
Endotoxemia and Sepsis in Renal Injury- Pathophysiology
- Systemic Hypotension
- Direct venal vasoconstriction
- Activation of vasoactive hormones(RAAS and endothelin)
- Induction of Nitric Oxide synthase (vasodilation, diminish platelet aggregation)
- Cytokine release (TNF, interlukin 1, 6, chemokines
- Synthesis of Reactive oxygen Species
- Neutrophil activation
Intra-renal thrombus– Endotoxin-induced endothelial injury may predispose to intrarenal thrombus formation by directly promoting platelet aggregation. This occurs by diminishing the release of nitric oxide (endothelium-derived relaxing factor) that normally inhibits platelet aggregation and by increasing the synthesis of plasminogen activator inhibitor type 1, leading to a reduction in fibrinolytic activity.
Aminoglycosides– moderate degrees of volume depletion can increase the risk of renal failure in the presence of a nephrotoxin, such as an aminoglycoside antibiotic. In this setting, the impairment in cell energetics induced by the aminoglycoside increases the susceptibility to ischemic injury.
5) Is Covid- 19 Related to AKI ?
- Patients with suspected or confirmed COVID-19 may present with acute kidney injury (AKI) as part of their overall illness. In single-centered, retrospective, observational study from Wuhan, China- 52 critically ill adult patients with SARS-CoV-2 pneumonia were admitted to the intensive care unit (ICU) of Wuhan Jin Yin-tan hospital (Wuhan, China) between late December 2019, and Jan 26, 2020. The results of the study showed that AKI was reported in 25 to 29 percent of patients who were critically ill or deceased. Acute kidney injury was identified on the basis of serum creatinine needed renal replacement therapy. The incidence of AKI among patients who are were less severely ill is unknown.
- A study of 59 patients with COVID-19 found that 34% of patients developed massive albuminuria on the first day of admission, and 63% developed proteinuria during their stay in hospital. Blood urea nitrogen was elevated in 27% overall and in two-thirds of patients who died. Computed tomography scan of the kidneys showed reduced density, suggestive of inflammation and edema.
- Cheng et al. recently reported that amongst 710 consecutive hospitalized patients with COVID-19, 44% had proteinuria and hematuria and 26.7% had hematuria on admission. The prevalence of elevated serum creatinine and blood urea nitrogen was 15.5% and 14.1%, respectively. AKI was an independent risk factor for patients’ in-hospital mortality.
Pathophysiology
- AKI is more common among patients with more severe disease, particularly in the ICU setting, and considered a negative prognostic factor with respect to survival.
- Conventional wisdom suggests that a maladaptive systemic inflammatory immune response, in the face of a cytokine storm, contributes to hypoperfusion-related injury of the renal tubules
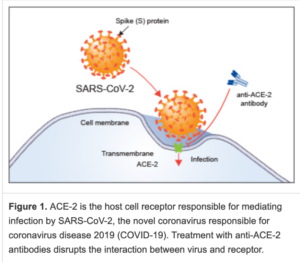
- In addition to organ dysfunction as a result of immune dysregulation, emerging evidence suggests the possibility of a direct cytopathic effect of SARS-CoV-2. ACE2and members of the serine protease family, essential for viral uptake by host cells, are highly expressed on podocytes and tubule epithelial cells.
Source:
https://www-uptodate-com.york.ezproxy.cuny.edu/contents/approach-to-the-adult-with-metabolic-acidosis?search=Approach%20to%20the%20adult%20with%20metabolic%20acidosis&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
https://www.kidney-international.org/article/S0085-2538(20)30251-9/fulltext
https://www.rndsystems.com/resources/articles/ace-2-sars-receptor-identified
https://en.wikipedia.org/wiki/File:Sepsis_Steps.png


