Cellulitis and Erysipela
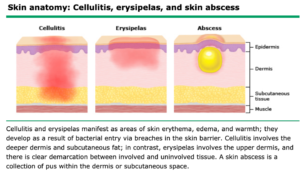
Cellulitis is an acute spreading infection of the deeper dermis and subcutaneous tissues. It may present with or without purulence, erythema may expand, lymphangitis( streaking) and septicemia may occur. Cellulitis is observed most frequently among middle-aged and older adults.

Patients with cellulitis may develop an abscess which is collection of pus within the dermis or subcutaneous space.

Erysipelas are a non-purulent superficial form of cellulitis that occurs classically on the cheek. Erysipelas have acute onset of symptoms with systemic manifestations like fever, chills, severe malaise and headache. Erysipelas have clear demarcation between the involved and uninvolved tissue described as a “sharply demarcated, glistening, smooth, hot plaque.” A classic description of erysipelas is “butterfly” involvement of the face.” Erysipelas occurs in young children and older adults.
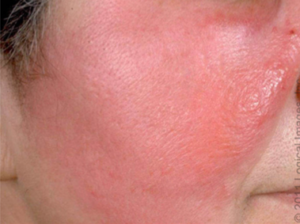
Millian’s ear sign is a distinguishing feature for erysipelas, since this region does not contain deeper dermis tissue

Cellulitis and erysipelas infections are nearly always unilateral, and the lower extremities are the most common site of involvement.

Etiologies/Microbiology
The most common causes of cellulitis and erysipelas are beta-hemolytic streptococci ( groups A,B,C,G and F), most commonly group A strep. Other common causes are Streptococcus pyogenes and S. aureus. Gram-negative aerobic bacilli and even fungi cause a minority of cases.
Diagnosis:
Usually based off clinical manifestations. Lab testing is not required for uncomplicated infections. Patients who develop abscess should undergo incision and drainage in the following circumstances.
- Severe local infection ( extensive cellulitis)
- Systemic signs of infection(fever)
- History of recurrent or multiple abscesses
- Failure of initial antibiotic therapy
- Extremes of age (young infants or older adults)
- Presence of underlying comorbidities (lymphedema, malignancy, neutropenia, immunodeficiency, splenectomy, diabetes)
- Special exposures (animal bite, water-associated injury)
- Presence of indication for prophylaxis against infective endocarditis
- Community patterns of aureus susceptibility are unknown or rapidly changing
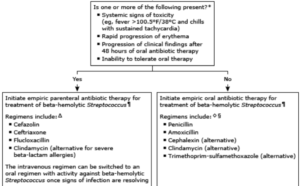
Treatment:
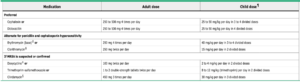
Cellulitis should be managed with empiric therapy for infection due to beta-hemolytic streptococci and methicillin-susceptible Staphylococcus aureus (MSSA).
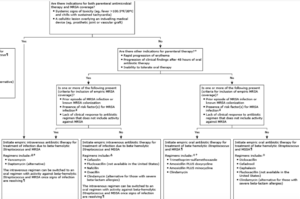
Erysipelas should be managed with empiric therapy for infection due to beta-hemolytic streptococci.
Impetigo
Impetigo is a highly contagious superficial bacterial infection of the skin. It is observed mostly in children ages two to five years but older children and adults can also be affected. Can be classified as primary impetigo which is direct bacterial invasion of previously normal skin. Secondary impetigo is infection at sites of minor skin trauma such as abrasions, insect bites, or underlying conditions such as eczema. Secondary impetigo is sometimes referred to as impetiginization.

There are three variations of impetigo: 1)non-bullous impetigo, 2) bullous impetigo, and 3)ecthyma..
- Non-bullous impetigo— Most common form. The lesions begin as papules that progress to vesicles surrounded by erythema. They eventually become pustules that enlarge and rapidly break down to form thick, crusts with a “golden appearance” within one week. Lesions usually involve the face and extremities.

- Bullous impetigo— a form of impetigo( primarily in young children) in which the vesicles enlarge to form flaccid bullae with clear yellow fluid. They later become darker and more turbid. Ruptured bullae leave a thin brown crust. Bullous impetigo in an adult with appropriate demographic risk factors should prompt an investigation for previously undiagnosed human immunodeficiency virus (HIV) infection.

- Ecthyma— This is a ulcerative form of impetigo. The lesions extend through the epidermis and deep into the dermis. They can be described as “punched-out” ulcers covered with yellow crust surrounded by raised violaceous margins.

Microbiology: S. aureus. (Most common). Beta-hemolytic streptococci (primarily group A) account for a minority of cases, either alone or in combination with S. aureus.
Diagnosis: made on the basis of clinical manifestations. Gram stain and wound culture.
Treatment: Bullous and non-bullous impetigo can be treated with either topical or oral therapy.
Topical (for limited skin involvement): Mupirocin TID, Retapamulin BID. Recommended length of treatment is five day
Oral (for numerous lesions):
Source:
https://www-uptodate-com.york.ezproxy.cuny.edu/contents/impetigo?search=impetigo&source=search_result&selectedTitle=1~122&usage_type=default&display_rank=1


