Paroxysmal Supraventricular Tachycardia(PSVT)
Supraventricular tachyarrhythmia is a narrow QRS complex (width <120 milliseconds or 3 boxes) tachycardia that arises above the bifurcation of bundle of His.
Pathophysiology:
Major causes: A reentrant circuit will go back to accessory pathway giving another electrical jolt, happening over and over again so HR will increase as atria is stimulated over and over again, producing a sustained reentrant tachycardia.
- AV node re-entrant tachycardia (AVNRT)- 60% percent of cases;
Two pathways within the AV node (1 nodal and 1 accessory)
- AV reciprocating tachycardia (AVRT)- 30 % percent of cases
- Atrial Tachycardia or Sino-atrial tachycardia- about 10 percent of cases

Diagnosis:
Electrocardiogram: regular narrow complex tachycardia w/ no discernable P waves due to rapid rate. Regular wide complex tachycardia mimicks ventricular tachycardia.
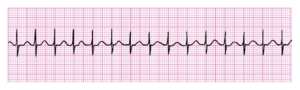
- Rate: 130 or higher.( commonly 140-250)
- Regularity: Regular.
- P waves: Not seen.
- PR: Not measurable
- QRS: <0.12 secs.
Treatment:
Valsalva maneuver — it induces a temporary slowing of SA nodal activity and AV nodal conduction by stimulating baroreceptors in the aorta. This triggers a reflex increase in vagus nerve activity and sympathetic withdrawal.
Carotid sinus massage- generally safe and well tolerated, but potential complications include profound hypotension and bradycardias, transient ischemic attack or stroke, and arrhythmia’s.
Adenosine: The usual initial dose is 6 mg( fast push), which can be followed by a maximal single dose of 12 mg if not successful. Repeated dosing beyond the 12 mg bolus is not usually effective.
———————————-
Atrial Fibrillation:
4 classifications
- Paroxysmal (ie, self-terminating or intermittent) AF –AF that terminates spontaneously or with intervention within seven days of onset. Episodes may recur with variable frequency.
- Persistent AF –AF that fails to self-terminate within seven days. Episodes often require pharmacologic or electrical cardioversion to restore sinus rhythm.
- Long-standing persistent AF (lone af)– AF that has lasted for more than 12 months.
- Permanent AF – term used to identify individuals with persistent atrial fibrillation x more than 1 year. Rhythm control strategy is the treatment.
Signs Symptoms
Palpitations, tachycardia, fatigue, mild dyspnea. More severe symptoms include dyspnea at rest, angina, presyncope, or infrequently, syncope. Not all patients with AF are symptomatic.
Pathophysiology:
- Numerous micro-reentrant circuits within the atria generate multiple waves of impulses which often compete with or even extinguish each other.
- no uniform activation of the atrial tissue and no distinctive P waves are generated or recognized on the surface ECG.
- Increase risk of atrial thrombus formation that can lead to cerebral and/or systemic embolization( stroke).

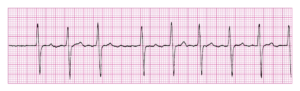

- Rate: Atrial—350–700, ventricular—varies depending on conduction.
- Regularity: Irregularly irregular.
- P waves: None. Wavy baseline between QRSs instead. Not discernable.
- PR: Not applicable.
- QRS: <0.12 secs.
Treatment:
– prevention of systemic embolization
– choice between a rhythm or rate control strategy
- Rate Control: drugs that slow conduction across the atrioventricular (AV) node, such as beta blockers( metoprolol, atenolol, esmolol), non-dihydropyridine calcium channel blockers( verapamil, diltiazem),or digoxin .
- Rhythm Control: Amiodarone, dofetilide, flecanide, propafenone, sotalol, and less common dronedarone
- Evaluate need of antithrombotic therapy: use CHA2DS2-VASc score
For non-valvular AF patients with a CHA2DS2-VASc score ≥2, there is a strong recommendation for oral anticoagulation. Non-vitamin K antagonist oral anticoagulants (NOAC), also referred to as direct oral anticoagulants, or DOAC) (eg,dabigatran,rivarobaxan,apixaban or edoxaban).These are chosen rather than warfarin for most patients in whom oral anticoagulant therapy is chosen.
—————————————
Heart Blocks
Atrioventricular (AV) block is defined as a delay or interruption in the transmission of an impulse from the atria to the ventricles due to an anatomic or functional impairment in the conduction system.
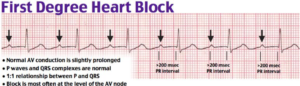
- Rate: Can occur at any rate.
- Regularity: Depends on underlying rhythm.
- P waves: Upright, matching, one per QRS.
- PR: Prolonged (>200 millisecounds) or 5 boxes.
- QRS: <0.12 secs.
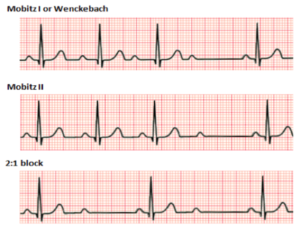
2nd degree block- Mobitz type 1 aka Wenckebach block
Mobitz type I second degree AV block can occur in patients with intrinsic AV nodal disease, myocarditis (including Chagas disease), acute inferior myocardial infarction or ischemia and cardiac surgery.
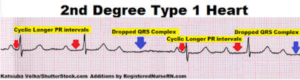

- Rate: Atrial—60–100, ventricular—varies.
- Regularity: Groups of beats, then a pause.
- P waves: Upright, matching, one blocked.
- PR: Gradually prolonging PR intervals until a QRS is dropped.
- QRS: <0.12 secs.
Tx:
Asymptomatic- no treatment
Symptomatic- atropine 1st line, epinephrine
Definitive is pacemaker is still symptomatic.
2nd degree block- Mobitz type 2
Treatment:
Unstable patients — temporary cardiac pacing.Atropine: initial dose of atropine is 0.5 mg IV. This dose may be repeated every three to five minutes to a total dose of 3 mg.
Stable patients — hemodynamically stable do not require urgent therapy with atropine or temporary cardiac pacing. Unstable frequently progresses to third degree (complete) AV block, so patients should be continuously monitored with transcutaneous pacing pads. Permanent therapy with an implantable pacemaker may be needed.
3rd degree block
AV dissociation– atrial (P waves) and ventricular (QRS complexes) are independent of each other.
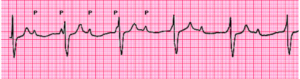
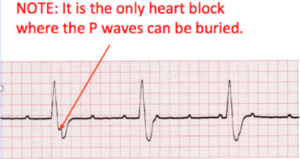
Treatment: transcutaneous pacing often followed by a pacemaker.
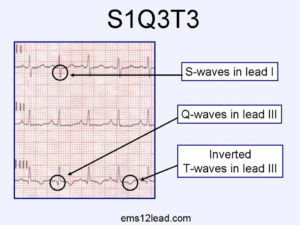
Pulmonary Embolism
The most common findings are tachycardia and nonspecific ST-segment and T-wave changes (70 percent). Abnormalities historically considered to be suggestive of PE (S1Q3T3 pattern, right ventricular strain, new incomplete right bundle branch block) are uncommon (less than 10 percent)

Source:
York College-Clin Med Slides
York College- Emergency Medicine Slides
https://www-uptodate-com.york.ezproxy.cuny.edu/contents/narrow-qrs-complex-tachycardias-clinical-manifestations-diagnosis-and-evaluation?search=svt&source=search_result&selectedTitle=1~91&usage_type=default&display_rank=1
https://www-uptodate-com.york.ezproxy.cuny.edu/contents/overview-of-atrial-fibrillation?search=afib&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
https://www-uptodate-com.york.ezproxy.cuny.edu/contents/etiology-of-atrioventricular-block?search=heart%20block&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2
https://www-uptodate-com.york.ezproxy.cuny.edu/contents/clinical-presentation-evaluation-and-diagnosis-of-the-nonpregnant-adult-with-suspected-acute-pulmonary-embolism?search=s1q3t3%20pattern&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2


